- Quantity: Measure the rate of the pulse (recorded in beats per minute). Count for 30 seconds and multiply by 2 (or 15 seconds x 4). If the rate is particularly slow or fast, it is probably best to measure for a full 60 seconds in order to minimize the impact of any error in recording over shorter periods of time. Normal is between 60 and 100.
- Regularity: Is the time between beats constant? In the normal setting, the heart rate should appear metronomic. Irregular rhythms, however, are quite common. If the pattern is entirely chaotic with no discernable pattern, it is referred to as irregularly irregular and likely represents atrial fibrillation. Extra beats can also be added into the normal pattern, in which case the rhythm is described as regularly irregular. This may occur, for example, when impulses originating from the ventricle are interposed at regular junctures on the normal rhythm. If the pulse is irregular, it's a good idea to verify the rate by listening over the heart (see cardiac exam section). This is because certain rhythm disturbances do not allow adequate ventricular filling with each beat. The resultant systole may generate a rather small stroke volume whose impulse is not palpable in the periphery.
- Volume: Does the pulse volume (i.e. the subjective sense of fullness) feel normal? This reflects changes in stroke volume. In the setting of hypovolemia, for example, the pulse volume is relatively low (aka weak or thready). There may even be beat to beat variation in the volume, occurring occasionally with systolic heart failure.
Blood Pressure: Blood pressure (BP) is measured using mercury based manometers, with readings reported in millimeters of mercury (mm Hg). The size of the BP cuff will affect the accuracy of these readings. The inflatable bladder, which can be felt through the vinyl covering of the cuff, should reach roughly 80% around the circumference of the arm while its width should cover roughly 40%. If it is too small, the readings will be artificially elevated. The opposite occurs if the cuff is too large. Clinics should have at least 2 cuff sizes available, normal and large. Try to use the one that is most appropriate, recognizing that there will rarely be a perfect fit.
Blood Pressure Cuffs


In order
to measure the BP, proceed as follows:
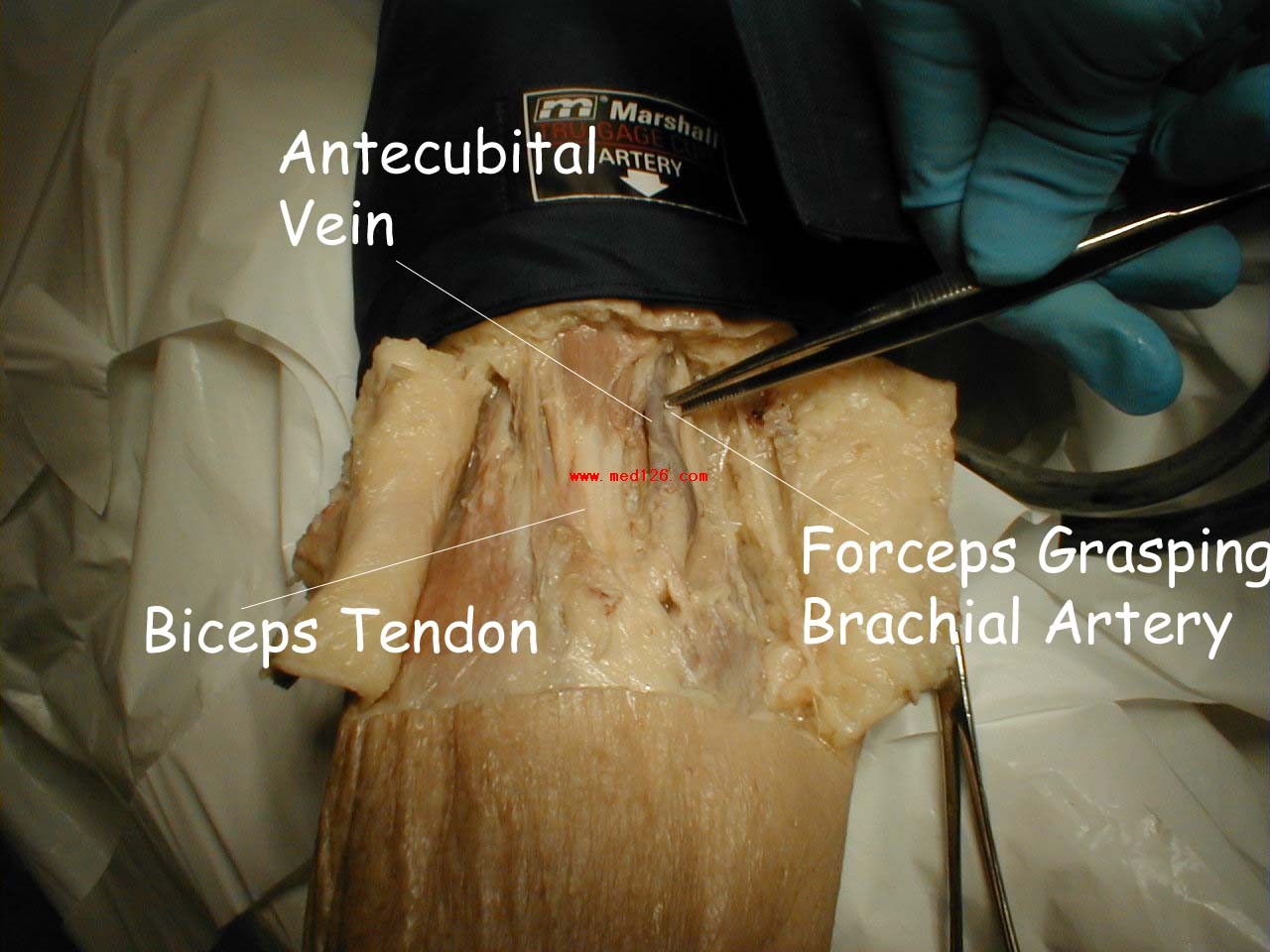
- Wrap the cuff around the patient's upper arm so that the line marked "artery" is roughly over the brachial artery, located towards the medial aspect of the antecubital fossa (i.e. the crook on the inside of their elbow). The placement does not have to be exact nor do you actually need to identify this artery by palpation.
Antecubital Fossa
The pictures below demonstrate the antecubital fossa anatomy (surface anatomy on the left, gross anatomy on the right).
- Put on your stethescope so that the ear pieces are angled away from your head. Twist the head piece so that the diaphragm is engaged. This can be verified by gently tapping on the end, which should produce a sound. With your left hand, place the diaphragm over the area of the brachial artery. While most practitioners use the diaphragm of the stethescope, the bell may actually be superior for picking up the low pitched sounds used for measuring BP. Experiment with both and see if this makes a difference. It's worth mentioning that a number of different models of stethescops are available on the market, each with its own variation on the structure of the diaphragm and bell. Read the instruction manual accompanying your stethoscope in order to determine how your device works.

- Grasp the patient's right elbow with your right hand and raise their arm so that the brachial artery is roughly at the same height as the heart. The arm should remain somewhat bent and completely relaxed. You can provide additional support by gently trapping their hand and forearm between your body and right elbow. If the arm is held too high, the reading will be artifactually lowered, and vice versa.
- Turn the valve on the pumping bulb clockwise (may be counter clockwise in some cuffs) until it no longer moves. This is the position which allows air to enter and remain in the bladder.
- Hold the diaphragm in place with your left hand. Use your right hand to pump the bulb until you have generated 150 mmHg on the manometer. This is a bit above the top end of normal for systolic blood pressure (SBP). Then listen. If you immediately hear sound, you have underestimated the SBP. Pump up an additional 20 mmHg and repeat. Now slowly deflate the blood pressure cuff (i.e. a few mm Hg per second) by turning the valve in a counter-clockwise direction while listening over the brachial artery and watching the pressure gauge. The first sound that you hear reflects the flow of blood through the no longer completely occluded brachial artery. The value on the manometer at this moment is the SBP. Note that although the needle may oscillate prior to this time, it is the sound of blood flow that indicates the SBP.
- Continue listening while you slowly deflate the cuff. The diastolic blood pressure (DBP) is measured when the sound completely disappears. This is the point when the pressure within the vessel is greater then that supplied by the cuff, allowing the free flow of blood without turbulence and thus no audible sound. These are known as the Sounds of Koratkoff.
Technique for Measuring Blood Pressure

- Repeat the measurement on the patient's other arm, reversing the position of your hands. The two readings should be within 10-15 mm Hg of each other. Differences greater then this imply that there is differential blood flow to each arm, which most frequently occurs in the setting of subclavian artery atherosclerosis.
- Occasionally you will be unsure as to the point where systole or diastole occurred and wish to repeat the measurement. Ideally, you should allow the cuff to completely deflate, permit any venous congestion in the arm to resolve (which otherwise may lead to inaccurate measurements), and then repeat a minute or so later. Furthermore, while no one has ever lost a limb secondary to BP cuff induced ischemia, repeated measurement can be uncomfortable for the patient, another good reason for giving the arm a break.
- Avoid moving your hands or the head of the stethescope while you are taking readings as this may produce noise that can obscure the Sounds of Koratkoff.
- You can verify the SBP by palpation. To do this, position the patient's right arm as described above. Place the index and middle fingers of your right hand over the radial artery. Inflate the cuff until you can no longer feel the pulse, or simply to a value 10 points above the SBP as determined by auscultation. Slowly deflate the cuff until you can again detect a radial pulse and note the reading on the manometer. This is the SBP and should be the same as the value determined with the use of your stethescope.
上一頁 [1] [2] [3] [4] 下一頁